-
United States -
United Kingdom -
India -
France -
Deutschland -
Italia -
日本 -
대한민국 -
中国 -
台灣
-
-
產品系列
查看所有產品Ansys致力於為當今的學生打下成功的基礎,通過向學生提供免費的模擬工程軟體。
-

Congenital heart defects (CHDs) are the most common types of birth defects, affecting nearly 40,000 newborns per year in the United States. Thankfully, nearly all children with simple defects survive into adulthood and lead normal lives. But about 1 in 4 of those children have more complex CHDs that require surgical intervention. There are many kinds of CHDs with many anatomical variations, meaning the surgical plan is different for nearly every patient. Understanding the intricacies of every individual patient’s heart is essential for positive outcomes.
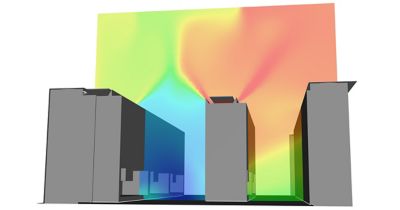
Cardiac surgeons usually use two-dimensional imaging tools such as echocardiograms, cardiac computed tomography (CT) scans, and magnetic resonance imaging (MRI) for preoperative planning. While great diagnostic tools, they have limited three-dimensional visualization capabilities. Surgeons only see the 3D, or in fact 4D, details of the heart when the patient is on the operating table, leaving little room to plan and perform a perfect reconstruction.
The Boston Children’s Hospital Cardiovascular 3D Modeling and Simulation Program, co-directed by Dr. David Hoganson and Dr. Peter Hammer, has created and institutionalized a standard of preoperative planning using 3D simulation tools so surgeons can have multiple types of visualization and prediction before entering the operating room. Their team of engineers and doctors create patient-specific 3D models of the heart and blood vessels for preoperative planning and intraoperative guidance.
“Making the best treatment decision really comes down to that individual patient and their specific anatomy and physiology,” says Hoganson. “We put together a team to use modeling and simulation in congenital heart disease to better understanding and predicting what operations and treatments would be best for individual children.”
Clinical use of computational flow modeling to determine the best approach for Fontan or Fontan revision
The A-Team Merges Engineering and Surgery
As a double board-certified cardio-thoracic surgeon, Dr. Hoganson’s clinical focus is on newborns and children with congenital heart disease. But he started his educational journey with engineering. “So, I’m really an engineer. My degree is in electrical engineering, and I developed devices for interventional cardiology and cardiac surgery,” he says. “During my surgical residency I did three years of full-time research at Massachusetts General Hospital and did a fair bit computational dynamics there.”
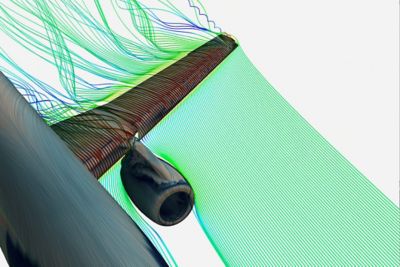
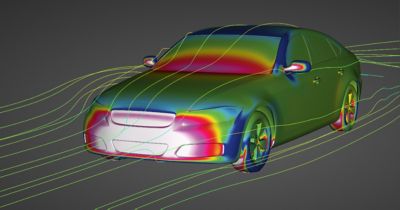
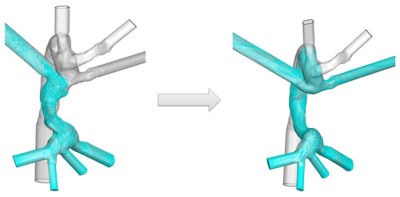
After completing his education and training, he joined Boston Children’s Hospital, where he and Hammer created the modeling and simulation program in 2018. Dr. Hammer is a mechanical engineer with over two decades in cardiovascular modeling. “Initially, we focused on computational fluid dynamics (CFD) in children with congenital heart disease and now also plan things like patches or new vessels that are created during these repairs,” he says.
The program has grown tremendously, in part because other clinicians are interested in using 3D models to help plan and conduct operations. For example, it is now a standard of care at the Benderson Family Heart Center to create patient-specific 3D models to help cardiac surgeons and cardiologists make preoperative plans for many CHD diagnoses. Their team of 12 includes multiple engineers who focus on CFD using Ansys Fluent and patient-specific 3D models using a host of different simulation tools, including Ansys Discovery.
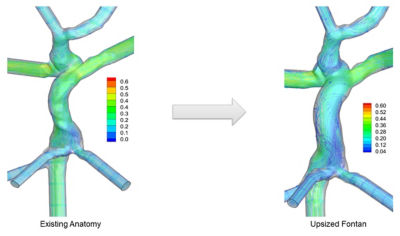
Modeling to optimize conduit size
Helping 1,000 Children, One Patient at a Time
Hoganson and his team have created over 1,000 patient-specific 3D models of hearts with a CHD. That’s more than 1,000 children that have been impacted by this work.
“Anytime you do simulation, it’s essential that you validate the work and confirm the simulation matched the clinical outcome,” says Hoganson. “So, for all our patients who have done CFD, we've done MRIs three to six months after surgery, so we know exactly how well the CFD model matches the outcome. This gives us great confidence that these simulations really tell the story of how the blood flow distributes, what the energy loss is going to be, and all these different important parameters.”
To ensure the models account for the different parameters as accurately as possible, Hoganson places particular importance on fine tuning boundary conditions that match individual patient physiology. “We build parameter models for the boundary conditions of individual CHD patients in Ansys Fluent and it’s a really seamless process,” he says. Using Fluent, Hoganson and his team can code outlet boundary conditions and parameter models. Then using physiologic information from the patient, they can fine-tune the parameter models so they have responsive boundary conditions that change over time depending upon different physiological states they’ve tested.
The results? Staggeringly similar CFD and MRI results.
Even so, there are and will always be biological variables that can’t be accounted for, but Hoganson and his team are taking every step they can to ensure the cardiac community trusts in their simulations. “We've been really thrilled with our results, but we're nowhere near a position to stop validating every single patient that we do. So, we've continued to do that and will continue to do that for the foreseeable future,” he says.
Accelerating the Process
Like most plans in life, things change, and surgical planning is no exception. Hoganson explains that using simulation for preoperative planning is an inherently iterative process that takes time to do.
“The first simulation we ever did took like three and a half months,” he says. “Now the entire iterative process of simulating multiple surgical options including all of the 3D modeling and virtual surgery work takes us around three and a half weeks.”
But the more complex the defect, the longer it takes. So the modeling and simulation team have used Discovery as a screening tool. Discovery gives them an initial 4D visualization of the defect before they do the full CFD simulation in Fluent.
“We’ve done well over 20 clinical CFD patients and not one single time have we done the CFD and then did the surgery that the surgeon had proposed,” Hoganson says. “One hundred percent of the time we have changed the operation based on the CFD results.”
“We’ve done well over 20 clinical CFD patients ... One hundred percent of the time we have changed the operation based on the CFD results.”
— Dr. David Hoganson, Co-director, Boston Children’s Hospital Cardiovascular 3D Modeling and Simulation Program
It’s Not Rocket Science, but It Is Heart Surgery
Pediatric cardiac surgeons spend roughly 12 years training to do these types of repairs. CHD patients and their parents only get a few months, or even weeks, to wrap their heads around a condition they may have never heard of and then try to understand how the surgeon is going to fix it. Hoganson uses the 3D simulation to explain to patients and their parents how the surgical team will approach their specific defect.
“These simulations have proven to be great communication tools. You don’t need a doctorate in engineering to look at a simulation and see where the flow is going,” he says. “The parents have a much clearer understanding of their child’s condition and how we are going to repair it.”
Simulation Can Mean the Difference Between Life and Death
Different departments within Boston Children’s Hospital have started to see the benefits of using 3D modeling and simulation and want in on the success. Hoganson and team recently helped create a model for an entire chest wall reconstruction.
Not only are others within the hospital interested, but other medical centers are as well. “We're working closely with several other leading centers in the U.S. and trying to help them get up to speed with some of the work that we're doing,” says Hoganson.
Dr. Hoganson and the rest of the modeling and simulation team are working hard to expand their capabilities and drive innovation for CHD patients.
“For every simulation patient, it’s life or death. This makes a big difference for every single child,” he says.
Learn more about Ansys solutions for clinical application engineering.
The Advantage Blog
The Ansys Advantage blog, featuring contributions from Ansys and other technology experts, keeps you updated on how Ansys simulation is powering innovation that drives human advancement.