ANSYS ADVANTAGE MAGAZINE
July 2021
How Does HVAC Airflow Influence Coronavirus Transmission?
By Lorenzo Mazzei, CFD Consultant, and Riccardo Da Soghe, CFD Branch CoordinatorErgon Research, Florence, Italy
The Vatican State Children’s Hospital was keen to minimize the risk of spreading COVID-19 in its waiting and treatment rooms. With the heat of summer approaching, facilities managers needed to know whether to turn on the air conditioning. Which was safer for patients: more airflow in closed rooms or less? Computational fluid dynamics (CFD) consultants at Ergon Research in Florence used Ansys Fluent to answer these questions.
Italy was hit early and hard by the novel coronavirus. By late March of 2020, the country was reporting an average of more than 6,000 new cases per day — a terrifying number at the time. A nationwide lockdown was implemented that month, which succeeded in reducing the number of daily new cases, but much of life in Italy did not regain any semblance of familiarity until May, when restaurants, bars and other gathering places were allowed to open again (though with strict social distancing protocols in place).
Living in lockdown during an Italian spring is one thing. One could live comfortably with neither the heat nor the air conditioning running. But in summer? Particularly in the south of Italy? Living or working in enclosed spaces without air conditioning could create a secondary health crisis that Italian hospitals very much wanted to avoid.
“Ergon Research’s simulations provided the Vatican State Children’s Hospital with the insights that administrators needed as the heat of Rome’s summer approached.”
For administrators at the Vatican State Children’s Hospital in Rome (the Ospedale Pediatrico Bambino Gesù, or OPBG, a premier pediatric hospital operating under the administration of the Vatican), this issue posed a serious operational question: Would turning on the heating, ventilation and air conditioning (HVAC) system in an enclosed hospital waiting or treatment room increase or decrease the risk of viral transmission to otherwise uninfected individuals? If an unmasked individual with COVID-19 coughed or sneezed — even if seated at an appropriate social distance from someone else — would uninfected individuals in that room be safer if the air were moving or still? Air that was not moving might keep viral droplets from spreading and infecting others. Then again, air that was moving might more rapidly diffuse viral concentrations and help move the droplets out of the room more rapidly.
In April of 2020, Dr. Luca Borro, an employee of the hospital, began asking questions in a Facebook group about using CFD to model a cough or sneeze event and simulating what would happen with the HVAC system running. Though Borro is an expert in 2D and 3D imaging, he was looking for support to deal with specific issues of the CFD modeling. He met Lorenzo Mazzei, a member of the group from Ergon Research, and that chance connection led to a collaboration in which CFD experts from Ergon Research volunteered their time and expertise to help the hospital find preliminary answers to these questions.
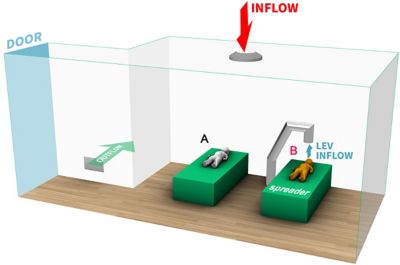
The model treatment room with one ceiling diffuser, one wall vent and an LEV inflow system
Developing A New Event Model: An Unmasked Cough
Ergon Research began life as a 2008 spinoff of the University of Florence. It provides consultative services in software development, experimental design and CFD, where its experts routinely use Fluent and Ansys CFX to help customers overcome complicated design challenges. Because Ergon Research was familiar with Ansys software and knew they could trust its accuracy, they elected to use Fluent to simulate the airflow.
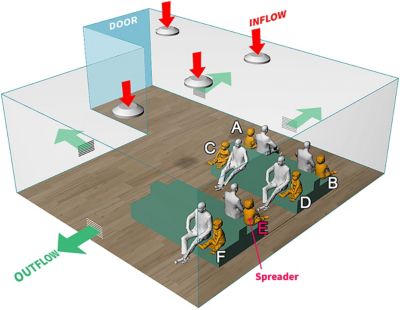
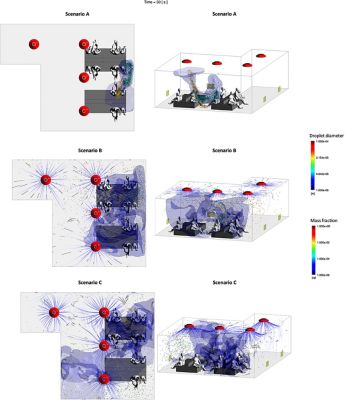
Borro and the team from Ergon Research started by constructing two CAD models — one of a waiting room and one of a treatment room. Into the waiting room model they placed benches for seats as well as a number of seated figures. Because the Vatican State Children’s Hospital is a pediatric hospital, the model included a balance of adult and child figures. The model also grouped the adults and children in pairs — as one might expect to find parents and children paired in a pediatric waiting room — and positioned the pairs, rather than the individuals, at the recommended 6-foot distance from one another. The waiting room model included four air diffusers in the ceiling, which would create a controlled positive airflow into the room when the HVAC system was operating, as well as four wall vents that would exhaust the air from the room. The treatment room model included a single ceiling diffuser, a single wall grate for exhaust and a specialized local exhaust ventilation (LEV) system positioned to draw air into a vent placed directly above the patient’s bed.
In many ways, these CAD models were deliberately simple. The ceiling air diffusers, for example, were generic, circular diffusers that included the deflectors in the simulation so as to solve the internal flow field rather than prescribing it on the boundaries. There were no features on the furniture because Ergon’s CFD experts knew that the inclusion of features such as chair arms, legs and backs would not have had a great impact on the informational outcome of the simulations they had planned. Moreover, they would have added considerably to the computational resources and time required to run the simulations. The physical features of the adults and children in the room were likewise simplified — though more detailed than the furniture — for the same reason.
All that was the easy part. The challenging part involved simulating the behavior of a cough occurring in these model rooms. Though the object libraries in Fluent are quite rich, they do not include pre-build models of a human cough. So, Ergon Research and OPBG created one from scratch. A search of the literature on the dynamics of a cough uncovered a 2018 doctoral dissertation on the numeric characterization of a human cough jet as well as a 1946 paper detailing the distribution of aerosolized droplets in a cough. The 1946 paper identified classes of droplets by diameter (from 3 μm to 750 μm), the respective number of droplets of each size class and the mass flow rate of each class of droplets.
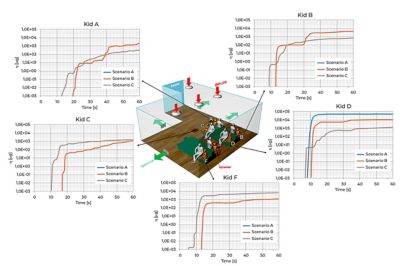
The x-y plots represent the temporal evolution of the index η, which describes the cumulative amount of contaminated air inhaled over time by different individuals in the room. Units are micrograms (μg).
Drawing on their experience in CFD simulations, the team at Ergon Research incorporated these event characteristics — along with droplet characteristics, the interaction of the aerosolized droplets with air molecules, and the buoyancy effects on both liquid particles and air due to gravity — into Fluent. Additionally, they incorporated models representing respiration/inhalation rates for each individual in the room, as well as models representing the mass fraction of the coughed air in the inhaled air (that is, the portion of contaminated particles contained in any inhalation after the cough event itself). The intent was to run coupled Eulerian-Lagrangian simulations to simulate a dispersion and potential for inhalation of aerosolized cough droplets within each of the room models they had built. Many of the key modeling components were already present in Fluent, such as particle injection and tracking, so there was no need to implement missing models. Additionally, Fluent had already been verified and validated against hundreds of papers analyzing Eulerian-Lagrangian simulations. Because Ergon Research wanted to use an event time step of 0.001 seconds and follow the movement of the aerosolized particles for a full 60 seconds, the team reduced complexity of the rooms’ CAD models to meshes of just 5M elements, which would conserve compute resources and time without compromising the clarity of the results they sought. They then ran a series of simulation scenarios using the waiting room model:
- Simulation A ran without any HVAC-mediated airflow
- Simulation B included airflow through the diffusers at a flow rate of 2020 m3/hr (the standard flow rate)
- Simulation C included airflow at a flow rate of 4040 m3/hr (double the standard flow rate
Ergon Research ran similar simulations on the model with the LEV system in the treatment rooms (with the LEV inlet vent positioned 43 cm above the spreader patient’s mouth and calibrated to exhaust air from the room at a rate of 1080 m3/hr). The solutions were obtained with a pressure-based solver and a semi-implicit method for pressure-linked equations (SIMPLE) algorithm with a second-order scheme for pressure and second-order upwind for all variables (except for turbulence quantities) while time was treated with a bounded second-order implicit scheme.
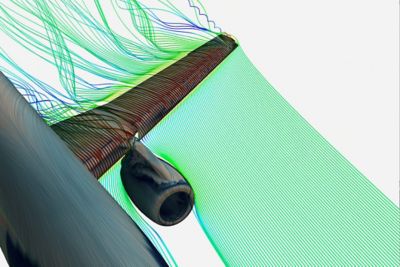
Increasing the flow rate of the HVAC system causes greater dispersal of less concentrated aerosolized droplets (view 2)
A Treatment Plan For The Hospital
The preliminary insights that emerged from Ergon Research’s simulations in Fluent were consistent, repeatable and somewhat surprising. In all the waiting room simulations, the aerosolized droplets larger than 100 μm tended to gravitate toward the ground (regardless of HVAC flow rate) while the smaller, lighter droplets dispersed through the room in different ways.
- In simulation A, involving no HVAC-mediated airflow, the lighter droplets moved directly toward the person sitting across from the person coughing (the spreader). Only the individual directly across from the spreader appeared to inhale any significant fraction (11%) of contaminated air.
- In simulation B, involving the normal HVAC flow rate of 2020 m3/hr, the lighter droplets expressed from the cough interact with airflow from the diffusers before they come into concentrated contact with the child sitting in front of the spreader and are rapidly dispersed through the room. This reduces the amount of contaminated droplets that the individual sitting directly across from the spreader might have inhaled if there were no airflow in the room (from 11% down to 2.5%), but it also disperses contaminated droplets more widely in the room and creates a slight opportunity for individuals to inhale those droplets. The contaminated droplets constitute 0.5% of the air that individuals farthest from the spreader might inhale.
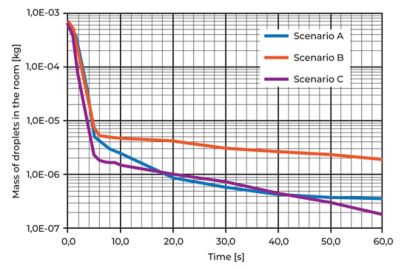
- In simulation C, in which the HVAC flow rate is doubled to 4040 m3/hr, the enhanced airflow wholly disrupts the aerosol cloud and quickly disperses it throughout the room. While this does expose individuals throughout the room to contaminated droplets, the increased turbulence both dilutes the concentration of contaminated droplets and increases the rate at which the wall vents pull the droplets from the room (at which point they no longer pose a risk to the individuals in the room). Thirty seconds after the cough event, those closest to the spreader are inhaling air that has only a 0.3% concentration of contaminated droplets, and those sitting furthest from the spreader are inhaling air that has only a 0.08% concentration of contaminated droplets.
- The treatment room simulations produced even more dramatic results: When the LEV positioned just above the patient’s head was engaged to draw air away from the patient at 1080 m3/hr, all infected droplets were pulled from the room within half a second of the spreader coughing, minimizing the likelihood of anyone in the room becoming infected from the droplets in the cough.
Increasing airflow reduces the mass of droplets in the room over time.
Ergon Research’s simulations provided the Vatican State Children’s Hospital with the insights that administrators needed as the heat of Rome’s summer approached. The outcomes derived through simulations in Fluent suggested not only that they should turn on the HVAC system in the hospital waiting rooms but that they should increase the airflow rate. At the doubled flow rate, air turbulence within the room could reduce the concentration of contaminated particles by 99.6% within seconds, thereby minimizing the likelihood that other patients would become infected from a cough. Similarly, use of an LEV system in a treatment room could minimize risk of exposure almost immediately. Administrators and health care personnel at the hospital would still have to fight an uphill battle against COVID-19, but at least they would not have to worry about complicating matters with a spike in patients suffering from heatstroke while sitting in overheated rooms.
시작하기
엔지니어링 과제에 직면하고 있다면우리 팀이 도와드리겠습니다. 풍부한 경험과 혁신에 대한 헌신을 가지고 있는 우리에게 연락해 주십시오. 협력을 통해 엔지니어링 문제를 성장과 성공의 기회로 바꾸십시오. 지금 문의하기