-
United States -
United Kingdom -
India -
France -
Deutschland -
Italia -
日本 -
대한민국 -
中国 -
台灣
-
Ansys stellt Studierenden auf dem Weg zum Erfolg die Simulationssoftware kostenlos zur Verfügung.
-
Ansys stellt Studierenden auf dem Weg zum Erfolg die Simulationssoftware kostenlos zur Verfügung.
-
Ansys stellt Studierenden auf dem Weg zum Erfolg die Simulationssoftware kostenlos zur Verfügung.
-
Kontakt -
Karriere -
Studierende und Akademiker*innen -
Für die Vereinigten Staaten und Kanada
+1 844,462 6797
ANSYS BLOG
October 5, 2018
Simulation Optimizes a Chemotherapy Implant to Treat Pancreatic Cancer
There are few illnesses as crafty as pancreatic cancer. It spreads like weeds and resists chemotherapy.
Pancreatic cancer is often asymptomatic, has a low survival rate and is often misdiagnosed as diabetes. And, this violent killer is almost always inoperable.
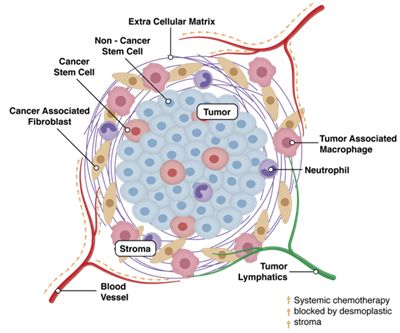
The pancreatic tumor’s resistance to chemotherapy comes from a shield of supporting connective tissue, or stroma, which it builds around itself.
Traditional chemotherapy can often be blocked by a tumor’s stroma.
Current treatments attempt to overcome this defense by increasing the dosage of intravenously administered chemotherapy. Sadly, this rarely works, and the high dosage is exceptionally hard on patients.
Nonetheless, doctors need a way to shrink these tumors so that they can surgically remove them without risking the numerous organs and vasculature around the pancreas.
“We say if you can’t get the drugs to the tumor from the blood, why not get it through the stroma directly?” asks William Daunch, CTO at Advanced Chemotherapy Technologies (ACT), an Ansys Startup Program member. “We are developing a medical device that implants directly onto the pancreas. It passes drugs through the organ, across the stroma to the tumor using iontophoresis.”
By treating the tumor directly, doctors can theoretically shrink the tumor to an operable size with a smaller dose of chemotherapy. This should significantly reduce the effects of the drugs on the rest of the patient’s body.
How to Treat Pancreatic Cancer with a Little Electrochemistry
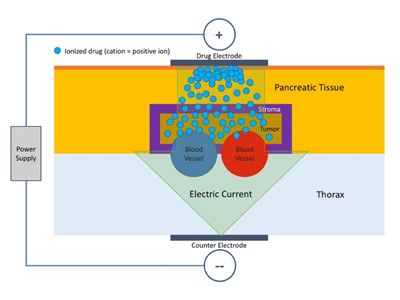
Most of the drugs used to treat pancreatic cancer are charged. This means they are affected by electromotive forces.
ACT has created a medical device that takes advantage of the medication’s charge to beat the stroma’s defenses using electrochemistry and iontophoresis.
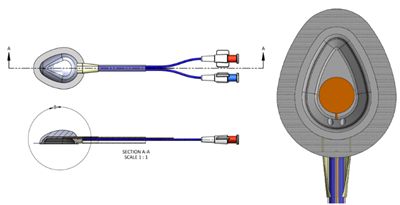
The device contains a reservoir with an electrode. The reservoir connects to tubes that connect to an infusion pump. This setup ensures that the reservoir is continuously filled. If the reservoir is full, the dosage doesn’t change.
Simplified diagram of the iontophoresis used by ACT’s chemotherapy medical device.
The tubes and wires are all connected into a port that is surgically implanted into the patient’s abdomen.
The circuit is completed by a metal panel on the back of the patient.
“When the infusion pump runs, and electricity is applied, the electromotive forces push the medication into the stroma’s tissue without a needle. The medication can pass up to 10 to 15 mm into the stroma’s tissue in about an hour. This is enough to get through the stroma and into the tumor,” says Daunch.
A diagram of ACT’s chemotherapy medical device.
“Lab tests show that the medical device was highly effective in treating human pancreatic cancer cells within mice,” added Daunch. “With conventional infusion therapy, the tumors grew 700 percent and with the device working on natural diffusion alone the tumors grew 200 percent. However, when running the device with iontophoresis, the tumor shrank 40 percent. This could turn an inoperable tumor into an operable one.” Subsequent testing of a scaled-up device in canines demonstrated depth of penetration and the low systemic toxicity required for a human device.
Daunch notes that the Food and Drug Administration (FDA) took notice of these results. ACT’s next steps are to develop a human clinical device and move onto to human safety trials.
Simulation Optimized the Fluid Dynamics in the Pancreatic Cancer Chemotherapy Implant
Before these promising tests, ACT faced a few design challenges when coming up with their chemotherapy implant.
For example, “There was some electrolysis on the electrode in the reservoir. This created bubbles that would change the electrode’s impedance,” explains Daunch. “We needed a mechanism to sweep the bubbles from the surface.”
An added challenge is that ACT never knows exactly where doctors will place the device on the pancreas. As a result, the mechanism to sweep the bubbles needs to work from any orientation.
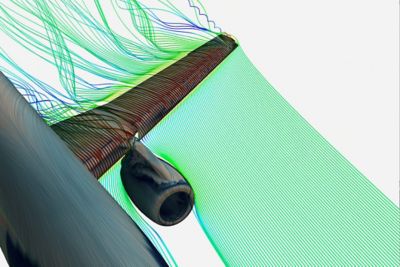
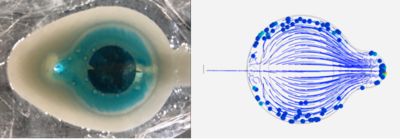
Simulations help ACT design their medical device so bubbles do not collect on the electrode.
“We used Ansys Fluent and Ansys Discovery Live to iterate a series of designs,” says Daunch. “Our design team modeled and validated our work very quickly. We also noticed that the bubbles didn’t need to leave the reservoir, just the electrode.”
“If we place the electrode on a protrusion in a bowl-shaped reservoir the bubbles move aside into a trough,” explains Daunch. “The fast fluid flow in the center of the electrode and the slower flow around it would push the bubbles off the electrode and keep them off until the bubbles floated to the top.”
As a result, the natural fluid flow within the redesigned reservoir was able to ensure the bubbles didn’t affect the electrode’s impedance.
To learn how your startup can use computational fluid dynamics (CFD) software to address your design challenges, please visit the Ansys Startup Program.