Heart disease is the leading cause of death for nearly every ethnicity in the U.S., affecting men and women alike, and it accounted for one-third of total global deaths in 2023. There are many types of heart disease, including arrhythmia, cardiomyopathy, coronary artery disease, and heart valve disease.
When heart disease is severe enough, it can lead to heart failure. Late-stage heart failure can result in a person needing a heart transplant. This procedure is the third-most common transplant in the United States — in 2023, 3,451 people received a new heart in the U.S. However, 4,298 people remained on the waitlist, and unfortunately, not everyone waiting on a new heart will receive one in time. But another option is now available: total artificial hearts (TAHs).
To encourage competition and innovation of TAHs, the Heart Hackathon was created in 2022 for university students around the globe. This yearlong competition offers students hands-on experience in researching, designing, and constructing a TAH, connecting them with industry experts while they develop technical, business, and professional skills. The inaugural winner, Team Bath Heart, hopes to repeat its success in the 2024 competition.
To the Beat of Your Own Drum
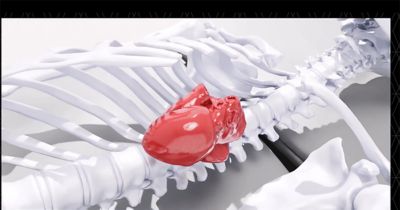
Think back to grade school, when you learned how the heart pumps blood. Oxygen-poor blood enters the venae cavae, flows through the right atrium and ventricle, then exits through the pulmonary artery, where it picks up oxygen in the lungs. Oxygen-rich blood re-enters the heart from the pulmonary veins, flows through the left atrium and ventricle, then exits through the aorta to the rest of the body.

Team Bath Heart (TBH)
The only TAH with worldwide regulatory approval, SynCardia, works in a similar manner, but it completely replaces the left and right ventricles with chambers connected to an external pneumatic driver system.
“An artificial heart is really just a mechanical pump,” says Katharine Fraser, senior lecturer at the University of Bath and faculty adviser to Team Bath Heart. There are many kinds of pumps for various liquids including turbines, positive displacement, and pneumatic, like the SynCardia TAH.
“The positive displacement method more closely mimics the natural heart, which is what the team is trying to do. We think we can create a long-term implantable positive displacement pump, which is softer and gentler on the blood,” says Fraser.
Blood is a sensitive liquid. Too much disruption can cause the cells to break down and not enough flow will cause them to clot, both of which are fatal.
Building on Previous Success
When the Heart Hackathon was announced in 2022, Team Bath Heart consisted of only six mechanical engineering undergraduates. By 2023, the team had grown to 30 students from various engineering disciplines, focusing on prototyping and testing work the 2022 team had started. They took their prototype to the International Society for Mechanical Circulatory Support (ISMCS) 2023 Conference for the inaugural Heart Hackathon finale, where they won first place. Today, there are nearly 70 students on Team Bath Heart, all hoping to repeat their success this fall in Japan.
“The competition is valued quite highly on novelty, and that’s one of the key reasons we won last year,” says Lucy Bilsborrow, integrated mechanical and electrical engineering student and technical team lead of Team Bath Heart. “We did a pumping method no other team — no other company making total artificial hearts — does.”
The team’s heart uses compressible bags located in the ventricles to pump blood throughout the body. A motor-powered mechanism contracts the bags, forcing blood out of the respective arteries.
To encourage innovative ideas, the Heart Hackathon TAH has surprisingly few technical requirements. The main requirement is the artificial heart must have a flow rate of at least five liters per minute delivered to both systemic and pulmonary circulations. Other than that, the size, materials, and powering mechanism are entirely up to the teams.
The team’s target demographic is a 49-year-old man who is 175 cm (almost 5 feet, 9 inches) tall and weighs 85 kilos (187 pounds). This is partially because older, heavier men are more likely to need heart transplants. This is also because decreasing the TAH size is one of the most difficult tasks the team has faced.
“The 2023 design was very large. For 2024 we reduced the size by 20%, but for an average female it needs to be even smaller,” says Molly Holmes, mechanical engineering student and testing lead for Team Bath Heart.
Working Out the Kinks
To address this and the other challenges the team is presented with, it uses a multitude of tools, including simulation.
“There’s a lot to get done in a short amount of time with very minimal funding,” says Fraser. “So from this perspective, simulation is really helpful because it lets the students explore different possibilities and ideas quickly without needing to physically create each prototype.”
Team Bath Heart has access to many simulation solutions through the Ansys Academic Program and Autodesk education plan, in addition to other solutions provided by the Hackathon itself.

Team lead Mansi Ahuja (left) and technical lead Lucy Bilsborrow (right) at a TBH stand at the vice chancellor’s garden party with the 2023, 2024, and 2025 total artificial heart (TAH) prototypes
“The Heart Hackathon gives us access to a company called Virtonomy. It basically offers this interactive replication of internal organs using real-life patient data,” says Holmes. “Then you can put your own computer-aided design (CAD) model inside that and see where the heart model is clashing with other organs and structures and where it attaches to blood vessels, which is really interesting.”
While Virtonomy lets team members visualize how the TAH will fit and connect within the body, they still have to design a working “heart.”
The casing of the heart is currently made of titanium. This strong material keeps the mechanisms inside the TAH from getting damaged, and it’s already been tested for biocompatibility by many existing medical device manufacturers. While titanium works great, the team is looking at other polymers to make the heart lighter, and the team uses the Ansys Granta EduPack set of teaching resources to do this.
“The casing material needs to fulfill the target specification, and we put these materials into the finite element analysis (FEA) solver for testing, and that speeds up the process without having to actually prototype it,” says Aaron Wong, mechanical engineering student and simulation lead for Team Bath Heart.
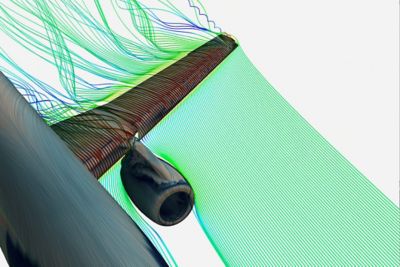
The team uses Ansys Mechanical structural finite element analysis software to analyze different stress points and, more specifically, cyclic stress. Just like natural hearts, TAHs need to beat, or pump blood, for as long as the patient lives. Team members use Ansys Fluent fluid simulation software and Ansys CFX computational fluid dynamics (CFD) software to simulate blood flow within the TAH valves. Due to time constraints, the team uses valves that are already on the market, but the team simulates the profile of each valve to determine which one works best with the TAH design.
“We did find out through CFX software that a polymer valve would produce less shear stress. That is one of the main things we test for in the blood flow because it’s really an important factor in contributing to hemolysis, which is one of the blood traumas we test for,” says Wong.

Rendering of the 2024 TAH casing in Autodesk Inventor
Through its design iterations, the team determined target specifications for blood trauma parameters, such as shear stress, Reynolds numbers, and flow rates. Performing different blood trauma tests helps meet the target specifications.
“We test for turbulence because you don’t really want turbulence in blood at high speeds, especially in a total artificial heart,” says Wong. “We also test for washout, which shows how much blood is retained after several cycles. So, a high washout will represent a better flow. It also indicates less stagnation points inside the design, because with stagnation, you might have blood clots and thrombosis.”
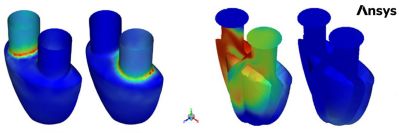
Wall shear stress (left) and washout (right) simulations of the 2024 TAH design
Not only is Team Bath Heart’s pumping mechanism unique, but so is its powering method. One of the biggest issues with artificial hearts is the electrical power delivery, which is typically made of cables stitched into the patient’s body through the thoracic cavity or abdomen. The risk of infection is high, and many patients complain that it is uncomfortable. It can also be inconvenient, as patients then have to carry around an external power supply, much like carrying around an oxygen tank.
“We want to transfer diagnostic data out of the heart with antennas and power it wirelessly,” says Ben Green, electrical engineering student and member of Team Bath Heart.
Green uses Ansys HFSS high-frequency electromagnetic simulation software to model how different bodily features, such as skin, muscles, and fat, will affect the antennas.
“The body has a huge impact on how antennas function,” says Green. “I can’t buy an off-the-shelf antenna and stick it in the heart. It won’t work. Different body tissues have different electric and magnetic properties, which will massively change the properties of an antenna and how they function, so we have to custom-design all our own antennas.”
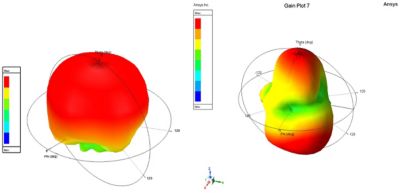
An antenna coil radiation pattern in free space (left) and an antenna coil radiation pattern in a simple phantom of transcutaneous layer (right)
Green also uses HFSS software to analyze absorption rates of the wireless power transfer system. To charge the heart, high power densities are passing through the patient, which poses the risk of the body absorbing that energy and producing heat. This ultimately harms the patient if warm enough.
“HFSS software allows us to look at the specific absorption rates so we can change our designs to maximize the magnetic fields and minimize the electric fields because the body doesn’t absorb magnetic fields — it only absorbs electric,” says Green.
With the help of academic supervisors, the team knows that there is a limit to the electrical power density that antennas can put out in the body. So, team members design all their antennas and wireless systems to be below that limit, with the goal of getting it as low as possible while still functioning to minimize heat.
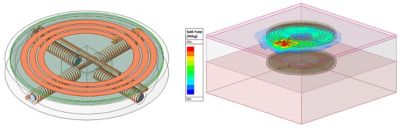
A wireless power transfer coil design (left) and a wireless power transfer coil specific absorption rate plot in a simple phantom (right)
The Benefits of Student Teams
The University of Bath is unique in that one of its largest student teams isn’t related to automotive. Many student teams at the high school and college level concentrate on cars, but the focus on healthcare is the biggest reason many of the students on Team Bath Heart decided to join. Some of the students and even the team’s advisers also appreciate the diversity the team brings.
“The students really wanted to make it a bigger thing because they wanted to attract diverse skill sets. But also, in terms of the types of people, it was very important to them that this was seen as something that anybody could take part in,” says Fraser. “We have all kinds of engineering disciplines, plus biology students, a couple of psychology students, and business students.”
With so many types of students from all different backgrounds, the Ansys Learning Hub and Autodesk education plan have helped the team strengthen its simulation skills.
“We don’t teach in-depth simulation until the final year. Many Team Bath Heart students are in their first and second years, so they overcome that challenge using the Ansys Learning Hub and by helping each other,” says Fraser.
The team also appreciates how integrated the tools from Ansys and Autodesk are, which makes it easier to rapidly generate and share ideas across the team.
“We had a lot of issues sharing files with each other because we're such a big team. We mentioned this to Autodesk, and they recommended we use Autodesk Fusion because everyone can work on the same project and it has version control,” says Holmes.
Autodesk even set up a whole training day for Team Bath Heart to help get it up and running on Fusion by transferring all its files and teaching some basics.
Ansys and Autodesk are rooting for Team Bath Heart to bring home another first-place win in the Heart Hackathon finale in Japan later this year.
Learn more about how an Ansys student team partnership and the Autodesk education plan can help your student team bring home the gold.
Just for you. We have some additional resources you may enjoy.
“There’s a lot to get done in a short amount of time with very minimal funding. So from this perspective, simulation is really helpful because it lets the students explore different possibilities and ideas quickly without needing to physically create each prototype.”
— Katharine Fraser, senior lecturer at the University of Bath and faculty adviser to Team Bath Heart