-
United States -
United Kingdom -
India -
France -
Deutschland -
Italia -
日本 -
대한민국 -
中国 -
台灣
-
Ansys is committed to setting today's students up for success, by providing free simulation engineering software to students.
-
Ansys is committed to setting today's students up for success, by providing free simulation engineering software to students.
-
Ansys is committed to setting today's students up for success, by providing free simulation engineering software to students.
-
Contact Us -
Careers -
Students and Academic -
For United States and Canada
+1 844.462.6797
ANSYS BLOG
April 26, 2024
Using In Silico Oncology to Defeat Pediatric Cancer
Dr. María Ángeles Pérez Ansón envisions a world without cancer, and she sees simulation as a key to making that vision a reality. If oncologists can simulate treatments on patient-specific digital models of cancerous tumors accurately, doctors could quickly choose the best therapy options and alleviate patient stress.
Pérez has been working on human body simulations for over two decades. Her 2004 thesis “Simulation of Cement Deterioration and Interfaces Debonding in Cemented Hip Implants” earned her a doctorate from the University of Zaragoza and subsequently won Best Technical Thesis of the year.
She is now a professor of structural mechanics at the University of Zaragoza’s department of mechanical engineering. She continues to work at the forefront of simulation technology as part of the Multiscale in Mechanical and Biological Engineering (M2BE) research group at the university’s Aragon Institute of Engineering Research.
The members of M2BE are experts in computational modeling, material strength, and structural mechanics. Instead of directing their expertise toward fields like architecture or aerospace engineering, Pérez and her team are exploring the intricacies of biological processes and the mechanobiology of cancer. They aim to enhance healthcare through advancements in tissue engineering, computer-aided diagnosis, and patient-specific modeling.
Ultimately, they hope these efforts will facilitate the establishment of a cloud-based platform to assist decision-making for cancer management and improve the planning behind the administration of therapeutics or surgical intervention.
A Pair of Formidable Foes
Pérez’s work closely relates to the PRIMAGE Project. PRIMAGE stands for PRedictive In-silico Multiscale Analytics to support cancer personalized diaGnosis and prognosis, Empowered by imaging biomarkers.
Financed by the European Commission, the project aims to develop ways to apply computational modeling and simulation (CM&S), or in silico, medicine to traditional medical imaging to evaluate and treat childhood cancers, specifically two types that, while rare, have higher mortality rates: neuroblastoma and diffuse intrinsic pontine glioma (DIPG).
DIPG is a type of brain tumor that occurs in the pons, a portion of the brainstem that controls much of the body’s unconscious vital functions like breathing, blood pressure, heart rate, and the sleep cycle. Only one to two children in 100,000 are diagnosed with DIPG each year. Unfortunately, mortality rates are very high. On average, 90% of patients with DIPG will die within the first two years of diagnosis.
Neuroblastoma, the focus of Pérez’s work with M2BE for the PRIMAGE Project, is a solid tumor that can appear anywhere in the body. Though rare, neuroblastoma is the most common form of solid cancer affecting children under five. Overall, the five-year survivability rate for high-risk cases is 50%.
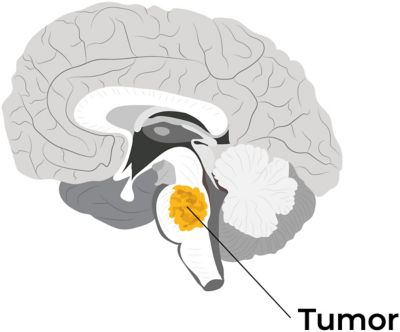
Diffuse intrinsic pontine glioma (DIPG)
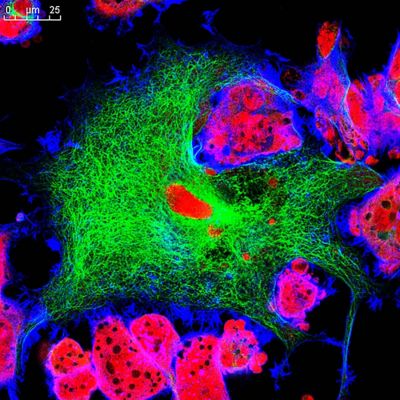
Fluorescence microscopic view of a neuroblastoma cell line in mice
For both types of cancer, researchers wanted to understand how effective a treatment would be before it’s even administered. With more targeted therapies, doctors could sidestep the risks of overtreatment and the subsequent health complications it may cause. M2BE’s work with simulation might eventually equip cancer researchers with that very ability.
“We are trying to reproduce a real physiological phenomenon and learn how a treatment could affect or modify the tumor’s behavior," Pérez explains. “The models we are creating could help the oncologist to decide which treatment or therapeutic strategy could be most appropriate for a certain patient.”
Developing a Digital Advantage
To build a digital model of a neuroblastoma tumor, M2BE drew upon their earlier work with bones and cells.
Previously, the team successfully modeled how human bones respond to mechanical loads and produced simulations demonstrating how skeletal tissue heals after fracture. They validated their models with in vitro laboratory work involving microfluidics and cell cultures. The team applied techniques derived from this experience to the development of multiscale computational models that can predict and simulate tumor growth and degrowth in response to treatment.
The simulation capabilities of Ansys products are fundamental to the research and experimentation that M2BE engages in at the University of Zaragoza. “Our analyses are extremely complex, and Ansys software allows a high level of customization and control.”
By leveraging the capabilities of Ansys Mechanical APDL and Ansys Workbench, the M2BE team took existing magnetic resonance imaging (MRI) data from a neuroblastoma scan and translated it to the basis of a digital model.
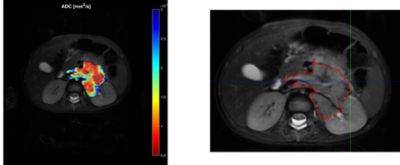
Magnetic resonance imaging (MRI) scan of a neuroblastoma
Different MRI sequences offer a detailed view of the body and tumor physiology. T2-weighted images (T2w) give the geometry of the organ or tumor. Dynamic contrast-enhanced (DCE) images offer detailed information about organ vascularization while diffusion weighted images (DWI) provide insight to the cellularity of the tumor. Armed with these details on their subject, the team set out to inform a working finite element (FE) mesh for their model.

Researchers took T2w-MRI slices and converted them to an .STL file to enable volumetric 3D meshing.
By stacking the T2w-MRI slices of the tumor, the team built a basic point cloud for the model, which was then converted to an .STL file — the same file type used in 3D printing — allowing for volumetric 3D meshing.
Next, to improve the foundation for the mesh and prevent potential convergence problems, the team smoothed the model’s geometry. Then, they integrated the clinical data on the tumor’s vascularity and cellularity, which essentially offered a roadmap of its interior vessels and a cell-by-cell blueprint of how it grew.
This allowed the team to create a patient-specific species diffusion model, or a more comprehensive model of the tumor that reflects its inner makeup and how fluids move through it.
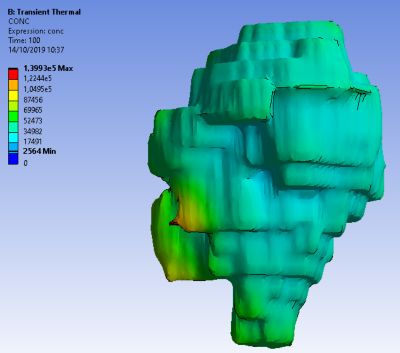
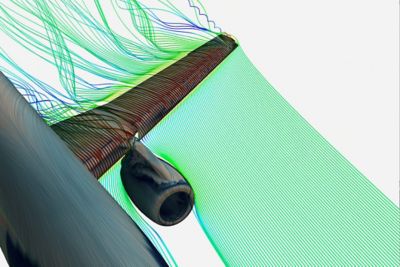
Species diffusion model
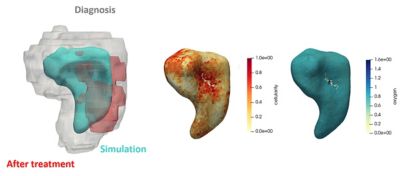
Finally, the team developed a patient-specific mechanical model of the tumor and the formulas that would govern its FE mesh. This model could simulate the cellular processes that occur during tumor growth. It could also respond to the availability of oxygen and nutrients or the introduction of chemotherapeutic drugs. These developments enabled the team to simulate the effect of a particular drug or its absence.
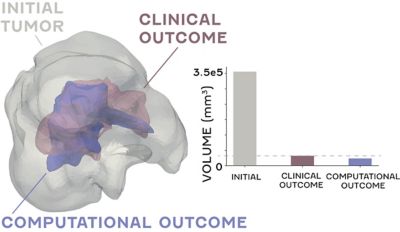
When applying their model to a clinical case, the team's predictions — derived from simulations of tumor growth and shrinkage on a patient-specific mechanical model — aligned with actual post-treatment outcomes, achieving roughly 90% accuracy. This promising initial result secured the validity of multiscale computational modeling for cancer research and set the stage for further development in the field.
Entering a New Era of Cancer Research
While Pérez admits that the models helping even 1% of cancer cases would be an incredible achievement, the significance of the progress already achieved by the group is undeniable.
By establishing the protocol for creating a digital model of a neuroblastoma, M2BE has opened the door for other researchers to do the same with all types of cancer. And with the advancements in digital engineering software making all this possible, it feels as though a global, cloud-based knowledge bank is possible. Suddenly, the notion of a cancer-free future doesn't seem all that far-fetched.
Learn more about how Ansys Mechanical and Ansys Workbench can help you with your healthcare innovations.